What is Bronchiectasis, and How is It Treated?
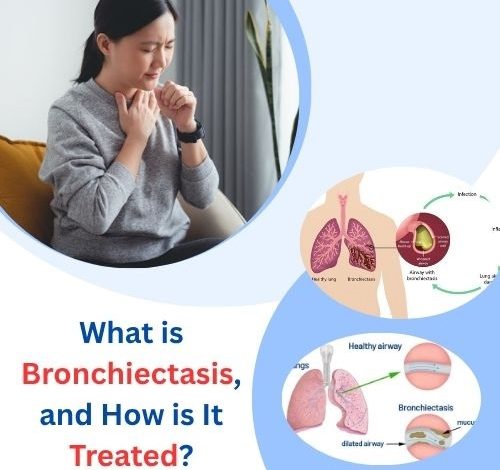
Bronchiectasis is a chronic respiratory disease that can have a significant impact on a person’s quality of life. While it is not as widely known as asthma or chronic obstructive pulmonary disease (COPD), bronchiectasis is a serious condition that demands greater awareness, early diagnosis, and appropriate management. This article provides a detailed overview of bronchiectasis—what it is, its causes, symptoms, diagnosis, and most importantly, how it is treated.
1. Bronchiectasis
Bronchiectasis is a chronic lung condition characterized by permanent widening and damage to the bronchi, the major air passages in the lungs. These damaged airways become flabby and scarred, making it difficult to clear mucus effectively. As a result, mucus builds up, leading to frequent infections and breathing difficulties.
The disease can be localized (affecting a part of the lung) or diffuse (affecting larger areas of both lungs). It can develop at any age and affects both men and women, although it is more commonly diagnosed in adults.

Related Article: Best and Worst Foods for Bronchiectasis: Eat Smart to Breathe Easier
2. How the Lungs Work: A Quick Refresher
To fully understand bronchiectasis, it’s helpful to grasp how healthy lungs function:
- Air enters through the nose or mouth, traveling down the trachea.
- The trachea branches into two bronchi, one for each lung.
- The bronchi further divide into smaller airways (bronchioles), eventually ending in alveoli, where oxygen exchange occurs.
These airways are lined with tiny hair-like structures called cilia, which help move mucus and debris out of the lungs. In bronchiectasis, these cilia are impaired, and mucus clearance becomes inefficient.
3. What Happens in Bronchiectasis?
In bronchiectasis, chronic inflammation or infection leads to structural damage in the walls of the bronchi. This damage results in:
- Widening of the airways (bronchial dilation)
- Thickened walls that impair airflow
- Mucus accumulation, which creates a breeding ground for bacteria
- Recurrent lung infections, which further damage the lungs
It becomes a vicious cycle: damaged airways lead to infections, which lead to more damage and worse symptoms.
Related Article: Natural Treatments for Bronchiectasis That Can Support Your Breathing and Wellbeing
4. Causes and Risk Factors
There are several underlying causes and risk factors for bronchiectasis, including:
- Post-Infectious Bronchiectasis
Many cases follow severe respiratory infections such as:
- Pneumonia
- Tuberculosis (TB)
- Whooping cough (pertussis)
- Measles
- Congenital Conditions
- Cystic fibrosis (CF): A genetic disease that causes thick, sticky mucus
- Primary ciliary dyskinesia (PCD): A disorder affecting cilia function
- Alpha-1 antitrypsin deficiency
- Autoimmune Disorders
Conditions such as:
- Rheumatoid arthritis
- Inflammatory bowel disease (IBD)
- Sjögren’s syndrome
- Allergic and Hypersensitivity Conditions
- Allergic bronchopulmonary aspergillosis (ABPA): A hypersensitivity to a common fungus
- Asthma (severe or poorly controlled)
- Obstruction
A foreign object, tumor, or enlarged lymph nodes can block a bronchus, leading to localized bronchiectasis.
- Immunodeficiency Disorders
Patients with weakened immune systems are more prone to lung infections.
5. Signs and Symptoms of Bronchiectasis
Bronchiectasis symptoms often develop gradually but tend to worsen over time. Common symptoms include:
- Chronic cough with daily sputum production (often thick and discolored)
- Recurrent chest infections
- Shortness of breath, especially during exertion
- Fatigue
- Wheezing
- Chest pain
- Clubbing (thickening of the fingertips in severe cases)
- Coughing up blood (hemoptysis) in some cases
The severity of symptoms can vary significantly between individuals.
Related Article: Fuelling Your Lungs: A Nutrition Guide for Bronchiectasis
6. Complications Associated with Bronchiectasis
Untreated or poorly managed bronchiectasis can lead to:
- Frequent and severe lung infections
- Lung abscesses
- Respiratory failure
- Collapsed lung (pneumothorax)
- Massive hemoptysis
- Heart complications (such as pulmonary hypertension)
Timely treatment and proper management are essential to reduce the risk of these complications.
7. Diagnosing Bronchiectasis
Diagnosis involves a combination of clinical history, physical examination, and diagnostic imaging. The steps include:
- Medical History and Symptoms
Doctors will ask about:
- Duration and frequency of symptoms
- History of lung infections
- Underlying medical conditions
- Physical Exam
May reveal:
- Crackles (rales) in the lungs
- Wheezing
- Clubbing
- Imaging Tests
The gold standard is a High-Resolution CT (HRCT) scan. It reveals:
- Dilated airways
- Mucus plugging
- Thickened bronchial walls
- Lung Function Tests
- Spirometry evaluates airflow obstruction
- Often shows a pattern similar to COPD
- Sputum Cultures
To identify bacteria or fungi responsible for recurrent infections.
- Blood Tests
To check for:
- Immune system deficiencies
- Autoimmune conditions
Related Article: Bronchiectasis: A Clearer Picture of Your Lung Condition
8. Treatment Options
Although bronchiectasis is not curable, it is manageable. The primary goals of treatment are:
- Clearing mucus from the lungs
- Treating infections
- Reducing inflammation
- Preventing complications
A. Medical Management
- Antibiotics
Used to treat infections and prevent their recurrence. Options include:
- Oral antibiotics (e.g., amoxicillin, azithromycin)
- Inhaled antibiotics (e.g., tobramycin)
- Intravenous antibiotics for severe infections
- Macrolides (e.g., azithromycin)
Have anti-inflammatory effects and reduce exacerbations.
B. Airway Clearance Therapies
- Chest Physiotherapy
Techniques include:
- Postural drainage
- Percussion and vibration
- Breathing exercises
- Devices
- Oscillatory PEP devices (e.g., Flutter, Acapella)
- High-frequency chest wall oscillation vests
These help loosen mucus and make it easier to cough up.
Related Article: 10 Powerful Bronchiectasis Remedies That Will Transform Your Breathing!
C. Bronchodilators and Steroids
- Bronchodilators
Used especially when coexisting asthma or COPD is present.
- Inhaled corticosteroids
Used to reduce inflammation, though their role is limited in bronchiectasis alone.
D. Vaccinations
Essential to prevent infections that can worsen bronchiectasis:
- Influenza vaccine (yearly)
- Pneumococcal vaccine
- COVID-19 vaccine
E. Surgical Options
Reserved for localized disease not responsive to medical therapy or life-threatening bleeding.
- Lobectomy: Surgical removal of the affected part of the lung
9. Lifestyle and Home Remedies
Lifestyle changes can significantly improve quality of life:
A. Hydration
Helps thin mucus and make it easier to clear.
B. Regular Exercise
Improves lung function and overall well-being.
C. Avoid Smoking
Smoking worsens lung damage. Complete cessation is essential.
D. Humidified Air
Using a humidifier may help with breathing and mucus clearance.
E. Nutritional Support
A balanced diet supports immune health.
Related Article: Foods to Avoid and Foods to Include in a Bronchiectasis Diet
10. Living with Bronchiectasis
A. Monitor Symptoms
Keep track of cough, sputum color, and breathlessness.
B. Regular Follow-ups
See your pulmonologist regularly and update your treatment plan.
C. Support Networks
Joining a support group can help manage the emotional toll of a chronic condition.
D. Recognize Exacerbations Early
Prompt treatment of flare-ups helps prevent hospitalizations.
Frequently Asked Questions (FAQs)
Q1: Is bronchiectasis the same as COPD?
No. They are distinct diseases but can coexist. Both affect airflow but have different causes and treatments.
Q2: Is bronchiectasis contagious?
No, bronchiectasis itself is not contagious. However, infections in patients with bronchiectasis may spread.
Q3: Can bronchiectasis be cured?
No, the lung damage is permanent, but symptoms can be controlled with Herbal Supplement for Bronchiectasis.
Q4: Is exercise safe for people with bronchiectasis?
Yes. Regular exercise helps with mucus clearance and improves lung capacity.
Q5: Can children get bronchiectasis?
Yes, although it is more commonly diagnosed in adults. Pediatric cases usually have an underlying cause such as genetic conditions or severe infections.
Related Article: Managing Bronchiectasis: The Power of Herbal Supplement for Bronchiectasis
Conclusion
Bronchiectasis is a complex, chronic lung disease that affects thousands worldwide. While it may not be as well-known as other respiratory conditions, its impact on daily life can be significant. With early diagnosis, consistent treatment, and lifestyle adjustments, many individuals with bronchiectasis can live active, fulfilling lives.
If you or a loved one has symptoms of chronic cough or recurrent respiratory infections, it’s essential to consult a healthcare provider. Early intervention can prevent the disease from progressing and improve long-term outcomes. Bronchiectasis may be a lifelong condition, but with the right management, it does not have to define your life.